Introduction
Cavitational osteonecrosis, also known as jawbone cavitions and NICO lesions were first described in the medical literature in 1920 by G.V. Black . They are are areas of hollow or dead bone. They rarely show up on x-ray and are normally totally painless. The condition is practically unknown by anybody in the health care field today whether doctor, dentist or surgeon. This makes trying to get it treated a significant challenge. A cavitation is actually a type of gangrene infection inside the bone. Just like in a gangrene infection, the only cure is to open up the area and remove the necrotic tissue. The immune system can not deal with this type of infection because there is no blood supply to effected area, leaving anaerobic bacteria free to multiply unhindered. The metabolic waste from the bacteria end up in the blood stream. The health implications from having this type of infection are profound.

[ Image Source: http://www.maxillofacialcenter.com/NICOxray/NICOxr2.html
The text from the website reads: "A rounded radiolucency posterior to the molar is so subtle that it is barely visible. It was a dry, hollow space or cavitation. The bur stops at the base of the lesion, which is as yet undisturbed except for the cortical window made to gain access."
How Common Are They?
In my own case, I had my lower two wisdom tooth removed and my root canal tooth. All 3 left cavitations so the surgeons that operated on me had a 100% failure rate. My mum had her lower wisdom teeth removed, both left cavitations, so she too experienced a 100% failure. In the paper Routine Dental Extractions Routinely Produce Cavitations dentists drilled into all old extractions sites, regardless of radiological appearence and found that 75% of extractions left cavitations. So this problem is clearly common.
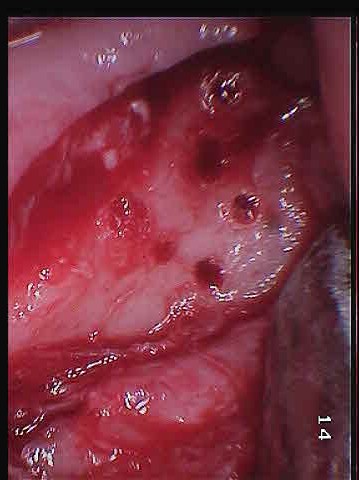
Cavitation Pictures
These next two images are my own surgery pictures. The first picture is with the gum retracted. You can see small holes in the bone. That is diseased bone. The second picture is with top cut off the bone. You can see there is just a giant hole that extends back into my jaw. I was actually awake during the surgery, and made sure my dentist took those pictures, specifically for this website.

These next two pictures are from the same dentist. They are the typical cavitations formed after the extraction of teeth. The text from the website reads:
"Bone exposed on flap retraction. Note the open defect in the bone some 20+ years after the extractions. The defect was directly under the fibrous attachment. "


The final picture is actually damage to the bone from a tooth that had a root canal. The type of infection/necrosis in the bone is identical to that of a cavitation. In this case the infection was directly effecting the nerve, causing that person to suffer with trigeminal neuralgia. Technically this is known as a NICO lesion (neuralgia-inducing cavitational osteonecrosis). Since this type of problem rarely shows up on x-ray, the solution often proposed to a patient is often to cut the nerve at the base of the brain to stop the pain.

Causes
Any kind of infection or abscess in the jaw can cause cavitational osteonecrosis. For me my worst problem was caused by how my lower wisdom teeth grew. Below is an x-ray of my original problem.

You can actually see visible bone loss under the tooth. This bone has been destroyed by infection. What you can't see is, infection has killed the bone in almost that entire area.
One of the main causes of jawbone cavitations is poor extraction done by dentists. Teeth aren't attached directly to the bone, they are held in by ligaments. These ligaments must be removed for the bone to heal properly. Sometimes they are pulled out with the teeth but that is not always the case. In the paper Routine Dental Extractions Routinely Produce Cavitations they describe the problem quite well.
Also called the periodontal or periodental membrane, its continued presence in the extraction site effectively prevents the adjacent bone from biologically recognizing that the tooth has been extracted. Bone cells are not going to proliferate spontaneously and migrate through a membrane intended by nature to define their growth limits. As long as the periodontal ligament remains intact, or largely intact, the underlying bone cells consider the tooth to be present, and no biological signal for bone growth is triggered. At the upper portion of the extraction site, however, where there is no periodontal ligament, osteoblastic bone activity does initiate, and a thin cortex of bone will heal across the hole. This cap of bone is rarely more than several millimeters thick.
Interestingly implant surgeons know this well. An implant surgeon I went to see showed me special tools they use to remove the periodontal ligament. Not only do they remove the ligament they often debride the entire socket to stimulate healing. From the website fordentists.com:
Once the tooth root has been extracted, it is imperative to thoroughly debride the socket walls. This is best undertaken with a surgical spoon curette. This part of the procedure should not be rushed; each area within the extraction socket needs to be curetted and all remnant periodontal ligament tissues removed from the socket walls. This has the added advantage of inducing some bleeding (increased vascularity) into the socket. Occasionally, you may note that the extraction sockets fails to show much in the way of vascularity (such as in the mandibular arch) and this may necessitate the need to use a very small round bur to carefully perforate the cortical place within the extraction socket. It is important to invoke bleeding into the socket as a good blood supply is required for good wound healing.
Why regular dentists also don't do this when they extract teeth is an interesting question.
Finding Cavitations
The reason this problem is virtually unknown today is because dentists are reliant on x-ray, and cavitations rarely show up on x-ray. There are however other ways they can be found. The simplest and most crude way of finding them is to press down on the bone where a tooth was extracted. If there is an area that is painful in response to pressure the likely hood is there is a cavitation there. I successfully found my own cavitations that way. What this method doesn't tell you though is how big the effected area is. It may be a lot larger than you realise.
One of the best tools is the cavitat ultra sound scanner. This is a special type of ultrasound that was made specifically for finding these types of problems in the jawbone. Unfortunately there are very few dentists in the world with these scanners, and worse still, the company was put out of business fighting legal costs. The device essentially measures blood flow in the jaw. Areas of bone that have no blood flow are either necrotic or hollow. The scans look like this:
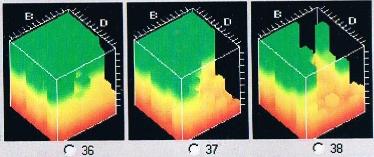
Green means healthy, areas of red are necrotic.
Since the company and it's website no longer exist, here are a few scans of the leaflet for the machine.
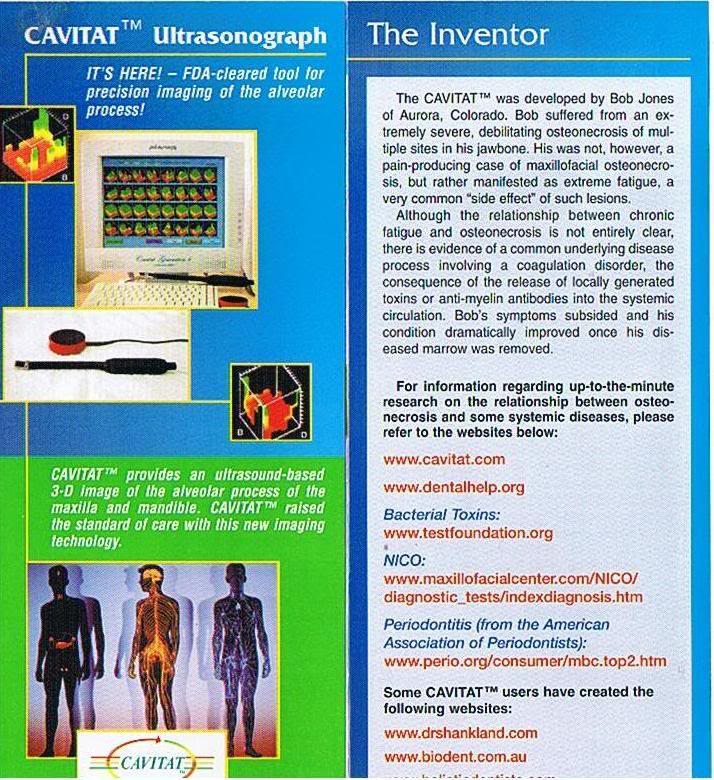

The cavitat machine can find problems that can not be found with any other tool avaiable today. However that being said it can miss problems. It missed one of my cavitations, which showed up quite happily on MRI, which leads me into the next section.
Since there are so few Cavitat scanners in the world, it might be impossible in some countries to find a dentist with one. Fortunately, these problems do show up on MRI. I went to my local doctor on the NHS, and he gave me a hospital referal and I was able to get one done at no cost. I only had to pay £10 for a digital copy of the scan. On my scans the cavitation showed up as a dark area. The first image the defect is circled. The second images is the same, but a deeper view inside the bone. You can see the shape of the lesion change as it goes deeper inside the bone. If you compare the circled side, to the other side you can see the difference.


This next image is an x-ray of the area where the bone defect was. It is not possible to see the defect on the x-ray, even though when it was opened up, it was large enough to stick your finger inside. Most dentists probably don't even realise x-ray is quite this limited, but it is.

CFS Connection
In my own case, after the lesion was operated on, after only a few weeks my energy started to come back and I started to feel like a human being again. Although I knew it was the metatolic waste from the anaerobic bacteria making me sick, the exact strains were not known. However after some hours of study I found that one of the toxins could be linked directly to chronic fatigue. Some anaerobic bacteria produce hydrogen sulphide. And according to wikipedia:
The toxicity of H2S is comparable with that of hydrogen cyanide. It forms a complex bond with iron in the mitochondrial cytochrome enzymes, thus preventing cellular respiration. Long-term, low-level exposure may result in fatigue, loss of appetite, headaches, irritability, poor memory, and dizziness
So amazingly this particular toxin starves cells of energy. And it is known that one of the main causes of CFS is mitochondrial failure.
Treatment
Just as in the removal of a a root canal tooth, all the infected bone from a cavitation site should be removed. The bone should be removed, if possible with hand tools. Hand tools are far less traumatic, and from a patient point of view far more tolerable. Drilling can fracture the bone microscopically and actually spread the infection. If done incorrectly it can also heat the bone too much impeding any kind of healing in that area. If drills are to be used by the dentist or sugeon, make sure it is a low speed drill, cooled with saline solution. Again implant surgeons would probably get this right, where your local dentist would not.
Sometimes the necrosis in the bone goes around vital teeth, and the only way to get at the infection is to remove that tooth. Failure to do so will see the infection come back. I lost two back molars because the the infection in the bone had totally destroyed the bone around the teeth. A third tooth the dentist manage to save, by trimming the root to get to the infection that wrapped around it. It is also important to understand that cavitation surgery no matter how well done it was can fail in time. The bone actually takes a surpisingly long time to heal. Originally I thought they would heal in something like a few months, but it turns out it can take closer to a full year. And in that time if infection gets back into that area, the cavitation can return. This happened to me on my largest cavitation, and so repeat surgery was required.
War Against The Truth
Jawbone cavitations exist in the medical literature. In fact the American Society of Endodontists prepared a statement on NICO lesions, in which their recommended treatment was surgical debridement. This hasn't stopped quackwatch from taking the makers of the CAVITAT to court, alleging the condition does not exist.

Other organisations such as the American Council on Science and Health have gone as far as to recommend that dentist that diagnose NICO should have their licenses revoked. These organisations are trying to make it very hard for people to get treatment. They are afraid of the cavitation diagnosis because it undermines the entire business model of a lot of dentists. We need to educate ourselves and fight back against these people, otherwise people who have what I have are going to die. Thankfully some informed people are fighting back.
Media
This is a lecture from one of the world leading experts on these problems.
Further Reading
www.drshankland.com
www.robertgammal.com
Beyond Amalgam: The Hidden Health Hazard Posed by Jawbone Cavitations
Maxillofacial Osteonecrosis & NICO
http://www.dr-lechner.de